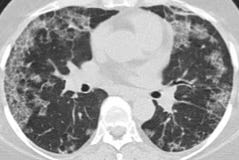
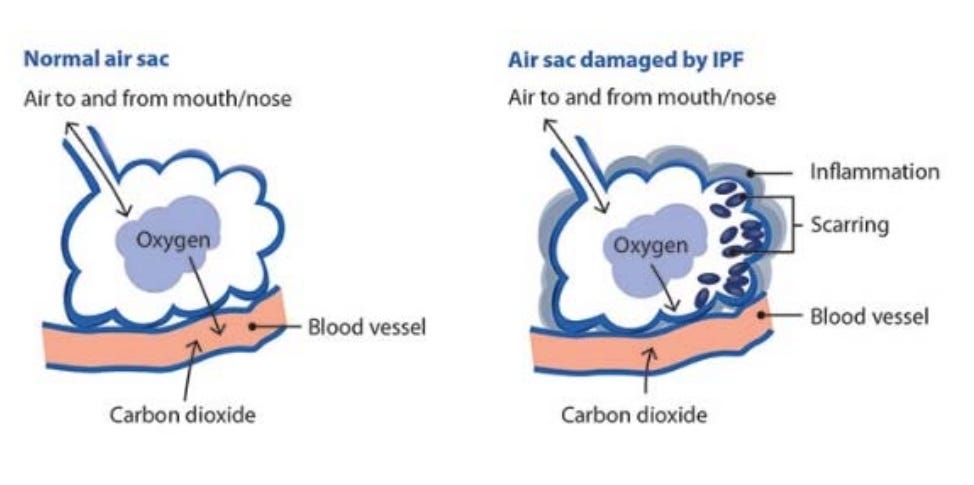
I was diagnosed with ILD – interstitial lung disease in January 2016. During my annual medical checkup in November 2015, I complained to the doctor that I had shortness of breath when I climbed a flight of stairs or exerted myself physically. I thought it was due to my lack of exercise! He put me on inhalers and asked me to report back if there was no improvement. There was none! So he referred me to a pulmonologist. The pulmonologist asked me to do a few tests, including a HRCT-high resolution CT scan. The results came back soon and during the visit with him, he gave us the news: fibrosis. I had never heard of this word before! It means scarring of the lung tissue where the alveoli become rigid and lose their function.
Being a researcher, I dug - hard. I learnt about ILD, UIP, IPF, NSIP, PF – the whole lot. There is a conference on Pulmonary Fibrosis in the US. I read all the papers and the videos. I cried. The prognosis was not good. The pulmonologist and the team could not decide whether it was IPF – idiopathic pulmonary fibrosis, or NSIP – non-specific interstitial pneumonia. That is a big deal because the prognosis for IPF is much poorer than NSIP. The doctor recommended a biopsy. I was reluctant, but what choice did I have? They did the biopsy. The results – inconclusive! Imagine your dilemma, 3-5 years or 10+ years. Not sure!
Then began solicitation for second, third, fourth opinions. One in the US, one in India, one in Bahrain, another in Saudi. Family and friends helped and prayed. No one was entirely sure. No clear diagnosis means no clear line of attack, medications and prognosis. Then we started researching the best hospitals that do research and are leading in this specific area of ILD. Mayo, Cleveland, Denver Jewish…were the top 3. I began soliciting referrals and finally ended up through some mutual family friend's daughter at Cleveland Clinic. We travelled to Cleveland and met with Dr. Parambil, a researcher pulmonologist at CC who has been working on ILD for some time
.
After more tests, and a review of the HRCT, lung biopsy results and consultations, he was sure that it was NSIP and not IPF. I had been given an 'extension'! He put me on specific medications of steroids and immuno-suppressants. Fast forward 3 years and I am still on the same medications. Was stable till November of 2018 when I caught pneumonia. 2019 start was not good and the numbers have deteriorated.
ILD - IPF, NSIP – do not strike the same fear as 'cancer'. But it is no different in terms of the disease impact. In fact the disease is very insidious – lurks and hidden in the back, with no external signs that there is an issue with the person. It is like a rotting apple core that looks perfect from outside! It is also a very grey disease. Diagnosis is very difficult and erratic. At least with cancer, people are sensitized. Not so with ILD!
The last three years have been tumultuous to say the least! You start looking at life differently. Your routine changes. Your attitude changes. You start thinking of what is important in life. Family. Time. Purpose. Giving back. Your bucket list. You come to a new normal. The brain is amazing. It has a fantastic way of coping. Once you get hurt, say a cut, the wound heals and there is a scar left. It is there but you forget about it. The same is true with the internal and mind wounds. It scars. Then you get used to it! You live with it – and it slowly eats away.
For my routine, medical checks and hospital visits have become the norm. You learn to wash your hands constantly, keep infections at bay. Avoid crowds and pollution. You sit home when it is dusty outside. You are paranoid about taking the flu shot and the pneumococcal vaccine. I have started to keep a log of my results, medications and progression. I schedule a visit to Cleveland Clinic twice a year. Monthly visits to the local hospital. Chatting with the nurse about the last PFTs – pulmonary function tests – even before the doctor has seen them. On the work front, giving back. I am close to retirement and have done well in my professional life. Received many a recognition. You start thinking about leaving a legacy. Training and coaching the young professionals. Passing on the wisdom to them. You want to spend more time with family. Take a trip to Japan with the girls, attend a wedding in Athens, meet friends in London, a trip to Ireland, then a family reunion in the US. Before it is too late to do it.
A diagnosis like this can feel like a restraining order but I have also found that this life change has brought with it an unexpected gift of sorts: liberation! Why me? used to come before. Not anymore! I have lived a great life and I am thankful for the time that is remaining. We raised two great girls who have both graduated, currently working, and are fiercely independent.
My personality type through the Briggs-Meyers test was an "INTJ" (Introverted iNtuitive Thinking Judging). An excerpt from the personality test interpretation:
INTJs are perfectionists, with a seemingly endless capacity for improving upon anything that takes their interest. What prevents them from becoming chronically bogged down in this pursuit of perfection is the pragmatism so characteristic of the type: INTJs apply (often ruthlessly) the criterion "Does it work?" to everything from their own research efforts to the prevailing social norms. This in turn produces an unusual independence of mind, freeing the INTJ from the constraints of authority, convention, or sentiment for its own sake.
In other words, we are control freaks. We ensure that things work properly. We plan ahead. We take care of the small details. Since the diagnosis, I have slowly seen a change in my personality. Starting to let go! Things will happen. You don't have to worry and it is ok if things don't as per plan! Was it overnight? No. I can still see some of its ugly head from time to time! It is a slow process. Here is a tip for research for the Briggs-Meyers team: Can a terminal disease change a person's personality?
I had always heard about living in the NOW. This has made me appreciate it and really live in the NOW. Learn to let go! Don't sweat the small stuff! I have learnt to say no. I have started yoga. Breathing exercises. Eating healthy. Don't worry about what people will say or how they judge you. Also learning to be less judgmental, less self-righteous, and more compassionate. Am I there yet? Absolutely not. But I have seen a trend in that direction.
I thought turning 60 would be a milestone in my life, but never did I see it coming this way. I used to think that I was untouchable, healthy, strong, powerful. I could fix anything. For that the universe gave me a hard kick in my ass!
Decisions come more easily with clarity and perspective, and things I'd previously weighted more heavily no longer matter as much. What does matter now is having family and friends and a wife who can be strong enough to shoulder this new responsibility with me. I look forward to simple things like golf and travelling (as long as I can). I am thankful that I am able to do these now. I'm getting to be okay with where I am now, receiving excellent care, having permission to slow down, and feeling like this happened for a reason. That reason was not something I could point to, control or plan, and maybe that was the whole point.
I feel like on that fateful day in January 2016 with my pulmonologist I entered a new world. Like in the movies. A world that was not known to me before. A world where I have discovered the inspiring people in the health care system. The professionals who are really good at what they do. I feel special and lucky to have the chance to be here. I used to feel suspicious of the drug companies. Now my attitude towards them has changed. While they are still-for-profit, they are doing their bit to find new medications and care. Most importantly, in this world there is hope! Hope for a cure, hope for arresting the disease, hope for a better prognosis. My pulmonologist says that my prognosis is very good. He points to his computer and the numbers and says that you will live to be 80! I have learnt that hope is a strong force.
During treatment, I learned about side effects of medications. Steroids are a miracle drug but has some serious side effects. It induces diabetes, and makes your face moon-shaped! Then you take drugs to tackle diabetes Those drugs make you feel achy and lethargic. Then you take Tylenol to fix the aches! It can become a never ending game. Medication balance combined with exercise and healthy eating is the call for patients like me! Or for anyone else. I am thankful that my side effects are not as severe as I have read in forums and support groups.
During this time, my family and friends have provided great support. I have also garnered it from Facebook forums specific for this disease. Some tips, some ways to manage and cope, from being in the same boat. I have always believed in God and my belief in Him has not wavered. What has changed is what a good friend told me once: from God- fearing, I have changed to God-loving. There is a difference!
I used to wonder how it would feel to be told I had a terminal disease. Watching those movies in the past, I used to cry. But that was it. It was happening to someone else. They were not my story. Once I was given the verdict, my initial reaction was the usual feelings anyone in this situation, or any other traumatic situation faces: fear, panic, sorrow, anger and all that other stuff. Then I found my resilience. I have learnt to face death and not be fearful of it! And to my amazement, I am handling it well. I am indeed stronger than I thought I could be. People say - be positive. Positive-ness is absolutely important. But I can’t will my fibrosis (scarring) away. I couldn’t tell my lungs to get back to their original self. I need to change my attitude, hope for a cure, and do the things on my bucket list!
I don’t want you to feel sorry for me. Not at all! I am thankful for spending some of my precious life with you, sharing memories, and your love. Let us celebrate the time we have together as much as we can!